Research
The Division of Molecular and Medical Genetics (DMMG) was generated in 2020, and we focus on the development of gene-addition/editing therapy including viral vector preparation and purification, adeno-associated virus (AAV) vector-mediated gene therapy for Duchenne muscular dystrophy (DMD), and anti-tumor gene therapy with lentiviral vectors. Our basic and translational efforts can allow producing new genetic therapies for various neuromuscular, hematologic, and metabolic diseases.
Development of new strategies for gene therapy
Development of gene therapy for hereditary diseases

Development of technologies using rAAV and their applications

Development of AAV vaccination
Features and challenges of AAV vaccines

Development of next-generation vaccines using AAV-related technologies

-
We are now developing novel variants of adeno-associated virus (AAV) vectors, that are expected to have high degree of safety and be capable of expression over longer periods of time, as well as basic technologies for their production and purification in order to achieve full-scale commercialization as gene therapy products.
We have also developed host cells with enhanced efficacy for vector production, and improved cell culture methods using bioreactors as well as the analysis of viral particles secreted into the medium are also under investigation. Regarding purification methods, in addition to the development of new ultracentrifugation technologies we are also promoting the creation of processes that combine ultrafiltration, ammonium sulfate precipitation, ion exchange, gel filtration and hydrophobic chromatography according to different purposes. To produce high-quality viral vectors that have minimal contamination with empty and incomplete particles, we are focused on the development of next-generation analytical techniques reflecting the guidelines of the FDA and domestic regulatory institutions, including the use of analytical ultracentrifugation and cryo-electron microscopy.
In addition, as a technology related to AAV vectors, we are also developing a non-viral DDS using hollow particles without the viral genome. While keeping the functional analysis of novel capsid mutants, we are also developing technologies to encapsulate or bind plasmids, DNA fragments or artificial nucleic acids to the empty particles and propose their application as nucleic acid therapeutics.
-
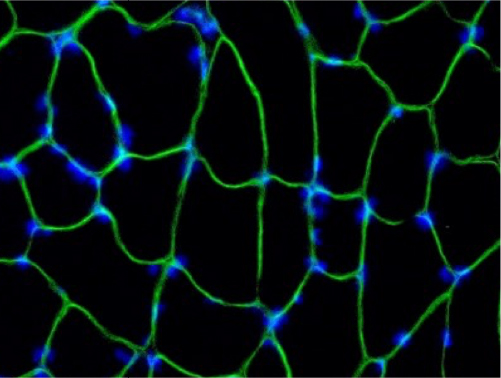
We are developing treatments for intractable neuromuscular diseases by applying vector-based technology to gene and cell therapies. To develop an effective treatment for Duchenne muscular dystrophy, for which there is no definitive treatment, we are verifying the safety and efficacy of the delivery of micro-dystrophin, and methods for the sustainable gene expression and induction of immune tolerance using mouse and dog disease model animals as well as primates.
-
Depending on the pathology and the genetic predisposition of the patient, stem cell therapy or a combination of gene and stem cell therapies may be beneficial. Because of this we are involved in the development of cell therapy technology in parallel with gene therapy. We are currently working towards the demonstration of the safety and efficacy of stem cell therapy for Duchenne muscular dystrophy and acute cerebral infarction in animal models of the disease. In the case of Duchenne muscular dystrophy, sponsor-initiated clinical trials began in 2023.
-
There is an urgent need for the discovery of biomarkers to be used for the evaluation of pathology in clinical trials, and we are conducting comprehensive analysis in animal models of Duchenne muscular dystrophy, resulting in the identification of many candidate compounds. Our aim is to combine clinical research with gene and cell therapy trials and to use the results to reach commercialization.
-
In response to the COVID-19 pandemic, and future infectious diseases that may become a threat, the “Program on R&D of New Generation Vaccine including New Modality Application” and the “Japan Initiative for World-leading Vaccine Research and Development Centers (Flagship Center)” has been launched and we are conducting research within the framework of the University of Tokyo Center for Advanced Infectious Diseases (UTOPIA), which has been selected as the base for these efforts.
We aim to apply our unique AAV vector-related technologies as a “Next-generation AAV Vaccine Modality (drug discovery method)” to commercialize safe and effective vaccines against both infectious and neurodegenerative diseases. AAV vectors are expected to be excellent vaccine modalities thanks to their stability and high immunogenicity. In addition, we are developing an efficient gene expression method that avoids AAV neutralizing antibodies and promote the development of new nucleic acid vaccines.
Our plans include the operation of a small-scale GMP manufacturing facility capable of producing viral vector vaccines at a scale that allows their use for clinical trials, operating it as a facility for research and manufacture of gene therapy vectors during normal times, allowing for the incorporation of the latest technologies and knowledge, and quickly and flexibly converting it into an early vaccine production facility in the event of an infectious disease outbreak, while at the same time contribute to the discovery and training of young researchers, which is the philosophy of UTOPIA.
-
We have developed vector-producing tumor-targeting cells by using stem cells that have the ability to accumulate in tumors. The cells are administered systemically and accumulate at cancer sites where they express the therapeutic gene, which is expected to result in enhanced efficacy against invasive and metastatic lesions where conventional anticancer drug or radiation therapies are ineffective.
-
In recent years, one of the ex vivo gene therapies, Chimeric Antigen Receptor (CAR)-T cell therapy, has been approved for refractory blood cell cancers, including leukemia, and its clinical use is increasing. CAR-T cells are genetically modified T cells that can bind and kill leukemia cells through the introduction of a CAR gene. Currently CAR-T therapy involves autologous transplantation, whereby T cells are extracted from the patient, the CAR gene is introduced and then the cells are subsequently returned to the patient. The most common method to introduce the CAR gene is through the use of lentiviral vectors. We are engaged in the development of next-generation cancer treatments that employ CAR genes and leverage on the lentiviral vector technologies that we have cultivated in our research for leukemia and cancer. Furthermore, lentiviral vectors, that allow long-term, stable gene expression, are attracting interest in the context of in vivo gene therapy for genetic disorders. In our laboratory, we are developing methods to produce lentiviral vectors that can be administered in vivo, taking advantage of our expertise in the optimization of AAV vector production.